A recent study reportedly identified typical parasites found in cat feces as a key discovery for potential treatments of illnesses such as Alzheimer's and Parkinson's.
According to Interesting Engineering, his new method, which uses a modified strain of Toxoplasma gondii, offers a fresh way to transport therapeutic proteins straight to the brain.
While still in the initial phases, the study provides an optimistic look at conquering a difficult obstacle in neurological medicine.
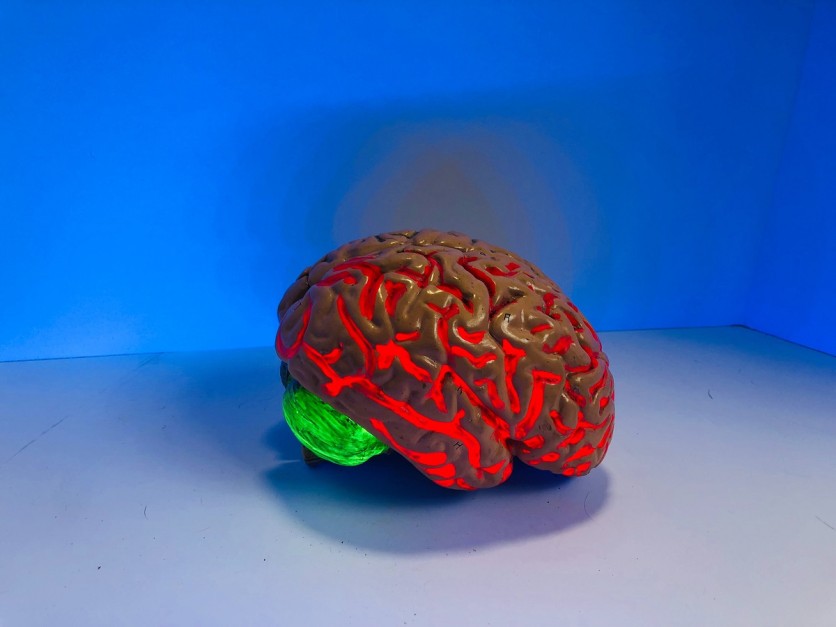
The difficulty of getting specific treatments through the blood-brain barrier and into precise neurons has been a persistent issue in neurological medicine. Toxoplasma gondii, a parasite commonly linked to feline excrement, has shown remarkable skill in crossing this barrier. This parasite naturally migrates from the gut to the brain, releasing proteins into neurons.
(Photo : Natasha Connell/Unsplash)
AI Software Can Detect Alzheimers at 95% accuracy
A group of global scientists, headed by the University of Glasgow and working with Tel Aviv University, have utilized this characteristic by modifying a form of Toxoplasma gondii to transport healing proteins.
This novel method focuses on the persistent challenge of reaching brain cells affected by disease, a critical factor in treating conditions such as Alzheimer's, Parkinson's, and Rett Syndrome.
The team concentrated on providing the MeCP2 protein, which is recognized for its promise as a treatment target for Rett Syndrome, a serious neurological condition resulting from mutations in the MECP2 gene.
The genetically modified parasites effectively generated and transported the MeCP2 protein to the proper place inside the cells in brain organoids and mouse models.
The study team observed that the parasite effectively generated the protein and subsequently transported it to the specific cell location in brain organoids and in mice models. This represents a major achievement in showing the promise of parasites for delivering neurological treatments.
Far From Application
Although groundbreaking, this method is still several years away from being implemented. The scientists intend to carry out more experiments to guarantee the parasites are modified to perish after releasing their cargo, reducing the chance of harm. This stage is essential to prevent further harm to cells and guarantee the treatment's safety.
The research introduces an innovative idea in the field of medical science, proposing that organisms that have evolved to control the brain could potentially be utilized for medical treatments.
According to the press release, Professor Oded Rechavi from Tel Aviv University mentioned the research's innovative aspect, explaining that evolution has already developed organisms capable of manipulating brains. He suggests that instead of duplicating efforts, "we" should observe and utilize these creatures' skills.
Alzheimer's Disease Treatment
About other emerging treatments for Alzheimer's disease, a mid-stage study focusing on Alzheimer's disease yielded mixed findings for Novo Nordisk's Victoza, a frequently prescribed drug for diabetes.
Even though the drug didn't improve brain metabolism as intended, it demonstrated potential in other areas, leading to hope for similar GLP-1 medications.
The pharmaceutical industry has spent years concentrating its Alzheimer's research on targeting amyloid plaques, the main characteristic of the disease. However, recent studies suggest that metabolic problems, such as insulin resistance and issues with processing glucose, could also contribute to cognitive decline.
This has resulted in a growing fascination with utilizing diabetes medications, like GLP-1 agonists, for managing Alzheimer's disease.
The research on Victoza, a GLP-1 agonist, examined how it impacts brain metabolism in 204 individuals with Alzheimer's disease. Sources reported that the drug did not show a significant improvement in this measure, but it did exhibit a decreased rate of cognitive decline and reduced brain atrophy in comparison to a placebo. These results indicate that GLP-1 drugs could have protective effects on the brain.

![Apple Watch Series 10 [GPS 42mm]](https://d.techtimes.com/en/full/453899/apple-watch-series-10-gps-42mm.jpg?w=184&h=103&f=9fb3c2ea2db928c663d1d2eadbcb3e52)



