The human papillomavirus (HPV) vaccine has emerged as an effective defender against cervical cancer, with a remarkable 65% decrease in incidence among women in their early 20s between 2012 and 2019.
This good news, however, is overshadowed by an alarming increase in cervical cancer rates among women in their 30s and 40s, indicating the need for increased awareness and targeted interventions.
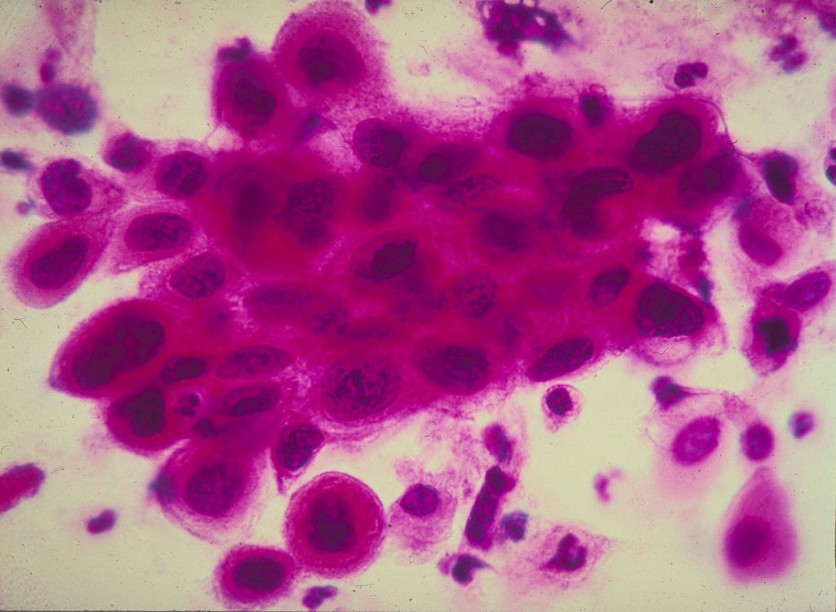
Cervical Cancer Cases See Alarming Trend
NBC News reports that decades of progress in the fight against cervical cancer, marked by a steady decline in cases and deaths, face a new challenge highlighted in a recent report by the American Cancer Society.
While rates have plummeted overall, concerns arise for women who were slightly too old for the HPV vaccination, with an almost 2% annual increase in cervical cancer diagnoses among those aged 30 to 44 from 2012 to 2019.
Dr. Nicolas Wentzensen from the National Cancer Institute underscores the significance of the HPV vaccine, affirming its role in the substantial drop in cervical cancer rates among women aged 20 to 24.
This generation, the first to benefit from the vaccine approved in 2006, has experienced a commendable 65% reduction in incidence.
Despite these achievements, the report sheds light on a concerning stagnation in the overall cervical cancer rate across all age groups. This stagnation prompts a closer examination of screening rates and the factors contributing to the increase in cervical cancer cases among women in their 30s and 40s.
The HPV Vaccine
Jennifer Spencer, an assistant professor at the Dell Medical School at the University of Texas-Austin, emphasizes the importance of not forgetting the generation that missed the HPV vaccination window.
Fortunately, the cancers detected in 30- and 40-something women are mostly early, curable tumors, according to Ahmedin Jemal, senior author of the abovementioned report.
The study refrains from delving into the specific reasons behind the rise in cervical cancer rates among older women. Jennifer Spencer suggests that screening rates could play a pivotal role. Screenings, crucial for early detection and intervention, allow the removal of precancerous lesions before they evolve into cancer.
However, more than half of women diagnosed with cervical cancer either have never been screened or have not undergone screening in the past five years, according to the Centers for Disease Control and Prevention.
The decline in screening rates becomes more apparent when the number of women aged 21 to 65 adhering to the latest screening guidelines fell from 87% in 2000 to 72%, as the National Cancer Institute reported.
Spencer's research reveals that women aged 21 to 29 are the least likely to be up-to-date on their screenings, with disparities linked to race, insurance status, residence, and sexual orientation.
Dr. Betty Suh-Burgmann, chair of gynecologic oncology for Kaiser Permanente Northern California, stresses the need for increased patient education.
The US Preventive Services Task Force recommends specific screening guidelines, including Pap smears for women aged 21-29 every three years and alternative options for those aged 30 to 65. However, changing guidelines and confusion among women and healthcare providers may contribute to declining screening rates.
Stay posted here at Tech Times.
Related Article : Research Unveils Immune Cells That Can Combat Cancer, Offering Potential Breakthrough Treatment
ⓒ 2025 TECHTIMES.com All rights reserved. Do not reproduce without permission.




